High-Stakes World of Insured Rehab
The most expensive real estate in the United States isn’t a penthouse in Manhattan or a beachfront lot in Malibu. It is the top four lines of a Google search result page.
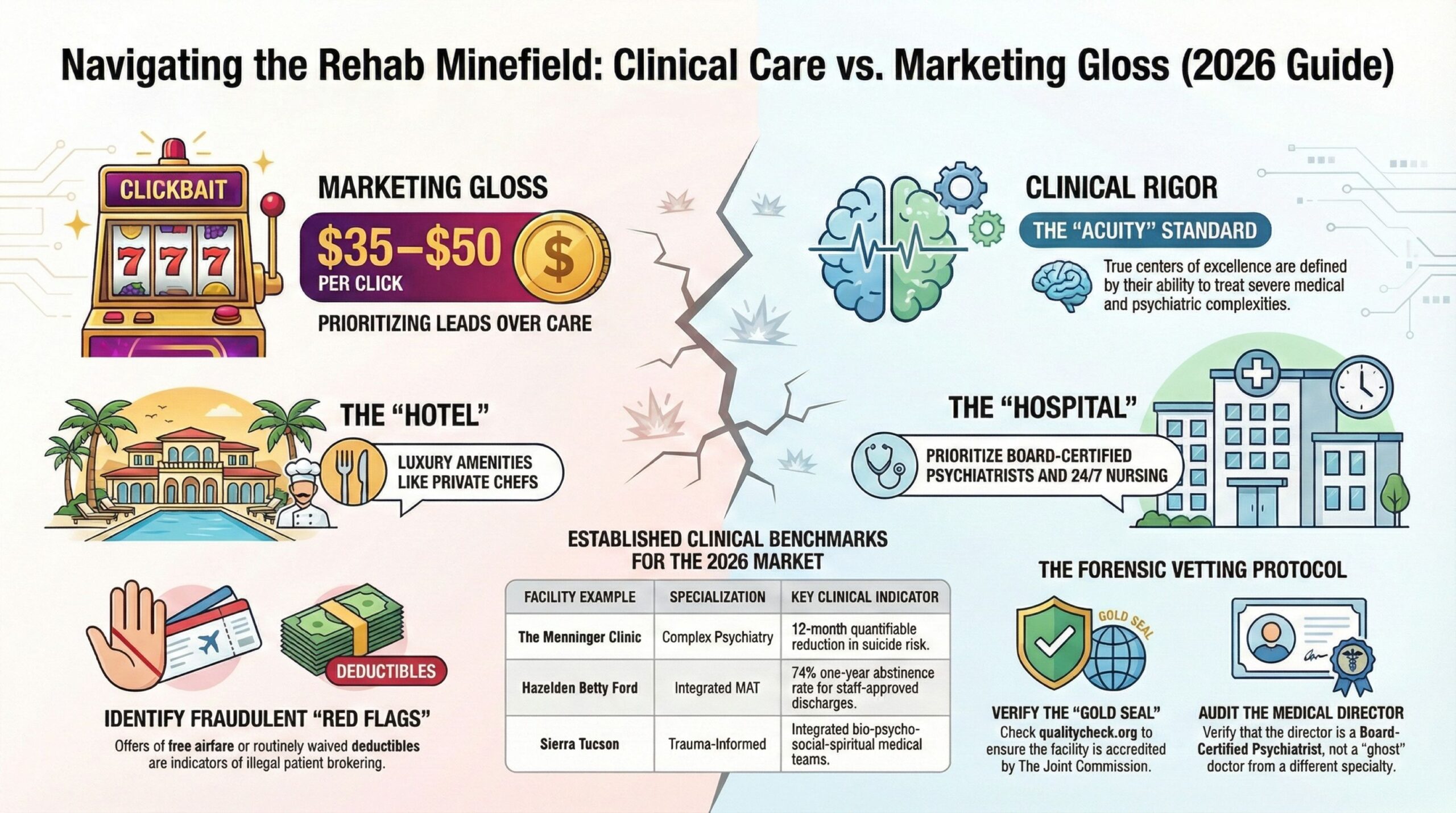
If you type “drug rehab for son” or “inpatient treatment accepts Cigna” into your browser right now, the companies appearing at the top of that list are paying an algorithmically determined ransom for your attention—often between $35 and $50 for a single click. In the addiction treatment industry, a desperate family is a “qualified lead,” and in 2026, the market for these leads is a multi-billion-dollar battlefield where clinical excellence often clashes with aggressive commerce.
We grounded this report in industry data from 2023 through 2025, looking closely at recovery research, accreditation standards, and market analysis. While we’ve worked hard to verify these numbers, the healthcare landscape changes fast. Rehab protocols and costs aren’t static. Consider this a solid baseline, but always double-check with a professional to get the latest specifics.
For the family member staring at a screen at 2:00 a.m., terrified by a loved one’s spiral into fentanyl or alcohol use, this digital marketplace is a minefield. The search results promise “Luxury,” “Cure,” and “100% Insurance Coverage.” The reality is a complex labyrinth of medical necessity criteria, out-of-network deductibles, and a disparity in care quality that can literally mean the difference between life and death.
This report investigates the intersection of high-quality clinical psychiatry and health insurance in 2026. We strip away the marketing gloss of “ocean views” to identify what actually works, how to pay for it, and where the true centers of excellence—like The Menninger Clinic in Houston or Hazelden Betty Ford—fit into a landscape often dominated by private equity.
The Landscape: “Luxury” vs. Clinical Rigor
To understand where to send a patient, one must first dismantle the marketing term “Luxury Rehab.” In the United States, this term has become a catch-all for facilities that charge premium rates (often $30,000 to $80,000 per month) but offer vastly different standards of care.
In 2026, the industry has bifurcated into two distinct models:
1. The “Malibu Model” (Amenities-Forward): These facilities prioritize the experience of recovery. They feature private chefs, equine therapy, and high thread-count sheets. While comfortable, many lack full-time, onsite medical staff. A physician might visit once a week to sign prescriptions, while the daily “therapy” is conducted by tech-level staff.
2. The Clinical Model (Evidence-Based): These institutions, often hospital-affiliated or non-profit, prioritize medical and psychiatric outcomes. The “luxury” here is not the thread count, but the presence of board-certified addiction psychiatrists, 24/7 nursing, and data-driven protocols.
The danger for the consumer lies in the blur. A facility with a generic website and an 800-number might look like a clinical powerhouse but operate like a resort with a loose medical license.
The Metric That Matters: Acuity
High-quality centers are defined by the acuity (severity) of patients they can safely treat. A standard “rehab” cannot handle a patient with liver failure from alcohol, a patient requiring IV medical detox, or a patient with co-occurring schizophrenia.
When vetting a facility, the first question should not be “Do you have a pool?” but “What is your medical capability?”
The Insurance Maze: ASAM Criteria and the “Fail First” Trap
In 2026, the battle for coverage is fought over the definition of “Medical Necessity.” Insurance carriers like Cigna, Blue Cross Blue Shield (BCBS), and UnitedHealthcare utilize specific guidelines to determine if they will pay for residential treatment.
The industry standard is the ASAM Criteria (American Society of Addiction Medicine). As of January 2025, many major carriers shifted to ASAM Criteria 4.0, a stricter, more integrated set of standards.
Understanding the Denial
Families are often shocked when an insurance company denies admission to a 30-day inpatient program, approving only “Intensive Outpatient” (IOP) care instead. This is not necessarily an error; it is a clinical determination based on risk.
To qualify for Level 3.7 (Medically Monitored Intensive Inpatient Services) or Level 4 (Medically Managed Intensive Inpatient Services) under most 2026 policies, a patient must demonstrate:
* Imminent Danger: A risk of severe withdrawal (seizures, delirium tremens) that cannot be managed outside a hospital.
* Biomedical Complexity: Co-occurring conditions (e.g., diabetes, hypertension, liver disease) that require 24-hour nursing.
* Failed Lower Levels: Documentation that the patient attempted outpatient treatment and relapsed (often called “Step Therapy” or “Fail First”).
The “Peer-to-Peer” Review:
When a denial happens, the facility’s doctor must get on the phone with the insurance company’s doctor to argue the case. Top-tier facilities have aggressive utilization review teams that fight these battles daily. Lower-tier facilities often accept the denial and attempt to flip the patient to “Cash Pay.”
Regional Spotlight: Houston, Texas
The Medical Heavyweight: The Menninger Clinic
While California and Florida dominate the search keywords, Houston, Texas, remains the quiet giant of psychiatric excellence. Anchored by the Texas Medical Center, this region hosts The Menninger Clinic, an institution that consistently defies the “rehab” stereotype.
The Clinical Difference:
Menninger does not market itself as a “vacation from addiction.” It is a specialty psychiatric hospital. Their data reveals that the average patient arriving at Menninger has already been hospitalized three times elsewhere. They specialize in the “complex” patient—someone with Bipolar I, severe personality disorders, and substance use issues simultaneously.
* Outcomes Data: Unlike most rehabs that rely on testimonials, Menninger publishes outcomes. Their 2024-2025 data sets regarding the “Compass Program” (for young adults) show significant, quantifiable reductions in suicide risk and improvements in emotion regulation that persist 12 months post-discharge.
* Insurance Reality: Menninger is in-network with select major carriers (including versions of Aetna and BCBS), but due to their high level of care, families often face a hybrid financial model. The “room and board” portion of the stay might be out-of-pocket, while the medical/clinical services are billed to insurance.
Why It Matters:
For a family dealing with a loved one who has “failed” three standard rehabs, a facility like Menninger represents a shift from “behavior modification” to “core psychiatric restructuring.”
Regional Spotlight: Rancho Mirage, California
The Gold Standard: Hazelden Betty Ford
In the saturated California market, where “body brokering” and ethical gray zones are rampant, the Hazelden Betty Ford Foundation (specifically the Rancho Mirage campus) remains the benchmark for integrity.
The “Cor-12” Protocol:
Hazelden was one of the first major legacy institutions to pivot away from strict “abstinence-only” dogma to embrace Medication-Assisted Treatment (MAT). Their “Cor-12” program integrates the use of buprenorphine (Suboxone) and naltrexone (Vivitrol) alongside Twelve Step facilitation. This is critical in 2026, as opioid use disorder outcomes are statistically poor without MAT support.
The Butler Center for Research:
Hazelden is unique in possessing an internal research institute. Their data is peer-reviewed and public.
* The Statistic to Know: Patients discharged with staff approval (completing the full clinical recommendation) have a 74% abstinence rate at one year.
* The Contrast: Patients who leave against medical advice (AMA) or are administratively discharged see that success rate drop below 45%.
Insurance Access:
Hazelden Betty Ford is aggressively in-network. They hold contracts with almost every major payer (Cigna, United, BCBS, Aetna). This accessibility makes them the primary “safe” choice for families who cannot afford a $60,000 cash-pay luxury center but require top-tier clinical care.
Regional Spotlight: Tucson, Arizona
The Integrative Model: Sierra Tucson
Consistently ranked #1 or in the top tier by Newsweek and Statista (2025 rankings), Sierra Tucson represents the successful merger of the “Luxury” setting with “Medical” rigor.
Located north of Tucson, this facility is known for its “Resident” model. Physicians and therapists work in integrated teams.
* The “Sierra Model”: They utilize a bio-psycho-social-spiritual approach. This includes aggressive testing for chronic pain issues, which often drive opioid addiction.
* The Niche: Sierra Tucson is particularly noted for treating trauma and PTSD alongside addiction. In 2026, the understanding of “Trauma-Informed Care” is non-negotiable. Addiction is rarely the primary problem; it is usually the solution to an underlying pain.
Insurance Note:
Sierra Tucson accepts many commercial insurance plans, but potential patients must verify “out-of-network” benefits. The high cost of their specialized trauma workshops often requires a detailed verification of benefits (VOB) prior to admission.
The Dark Side: Patient Brokering and The “Florida Shuffle”
No investigation into this industry is complete without addressing the predatory practices that plague the Google Search results.
The Scheme:
In states with high concentrations of rehabs (Florida, California, Texas), unscrupulous operators use “Patient Brokers” (sometimes called “Body Brokers”).
1. The Hook: A broker creates a generic website like “HelpForAddictionUSA.com.”
2. The Call: When you call, you aren’t speaking to a clinician. You are speaking to a closer in a call center who is paid a commission to “sell” your insurance policy to the highest bidder.
3. The Kickback: The treatment center pays the broker $500 to $5,000 for the patient.
4. The Cycle: To maximize insurance billing, the patient is cycled through unnecessary urine drug screens (billing $1,500 per cup) and then discharged to a “sober living” home owned by the same ring, only to be “relapsed” and re-admitted to restart the billing cycle.
Red Flags in 2026:
* Free Airfare: If a stranger on the phone offers to buy your son a plane ticket to Florida or California, hang up. This is a classic inducement used in brokering schemes.
* Waived Deductibles: It is illegal to waive insurance deductibles/copays routinely. If a center says, “Don’t worry about the $5,000 deductible, we’ll write it off,” they are committing insurance fraud, and your clinical care will likely be compromised to cover that loss.
* Generic Locations: If the website does not list a specific physical address (e.g., “Serving the Greater Houston Area” vs. “12301 Main St, Houston”), it is likely a lead-generation site, not a hospital.
The Vetting Protocol: How to Search Safely
If you are the person holding the insurance card, you have the power. Here is the forensic protocol for vetting a facility in 2026.
1. The Accreditation Check
Do not rely on the facility’s website badges. Go to the source.
* The Joint Commission (JCAHO): Search the facility name on JCAHO website. This is the same body that accredits major surgical hospitals. A “Gold Seal of Approval” is the baseline requirement.
* CARF (Commission on Accreditation of Rehabilitation Facilities): The alternative to JCAHO, focused specifically on rehab standards.
2. The Medical Director Audit
Find the name of the Medical Director on the facility’s “Team” page.
* Google their name. Are they a Board-Certified Psychiatrist or an Addiction Medicine specialist (ABAM)?
* Check the State Medical Board. Do they have disciplinary actions?
* The “Ghost” Doctor: In some scam facilities, the Medical Director is a retired proctologist or dermatologist lending their license. You want a psychiatrist.
3. The “Doctor-to-Doctor” Request
If you are dealing with a complex medical case (e.g., a patient with liver issues, history of seizures, or bipolar disorder), ask the admissions rep:
“Can my family doctor speak briefly with your Medical Director before we admit?”
A legitimate medical facility will facilitate this professional courtesy. A “churn and burn” rehab will refuse, because the Medical Director likely isn’t on site.
4. The Insurance Verification of Benefits (VOB)
Do not take the facility’s word that “You are covered.”
* Call the number on the back of your insurance card.
* Ask: “Is this facility In-Network or Out-of-Network?”
* Ask: “What is my maximum out-of-pocket responsibility?”
* Ask: “Do I have out-of-network mental health benefits?”
The Science of Recovery: What You Are Paying For
When the insurance company pays $20,000 or $30,000 for a month of treatment, what are they actually buying? In a high-quality facility, they are paying for Neuroplasticity.
Addiction is a chronic dysregulation of the brain’s reward system (specifically the dopaminergic pathways in the Nucleus Accumbens and the decision-making circuitry in the Prefrontal Cortex).
Effective treatment components in 2026 include:
1. Cognitive Behavioral Therapy (CBT) & Dialectical Behavior Therapy (DBT):
These are not just “talking.” They are skills-acquisition protocols. DBT, originally designed for Borderline Personality Disorder, is the gold standard for emotional regulation. It teaches the patient how to tolerate distress without reaching for a chemical solvent.
2. Pharmacotherapy (MAT):
* Opioid Use Disorder: Suboxone (Buprenorphine) or Methadone.
* Alcohol Use Disorder: Naltrexone (craving reduction), Acamprosate (brain chemistry stabilization), and Antabuse (deterrent).
* The Warning: If a rehab tells you “We don’t believe in drugs to treat drugs,” they are ignoring forty years of clinical evidence. This is a philosophical stance, not a medical one.
3. Family Systems Work:
While the individual carries the clinical label of “identified patient,” the family unit functions as the operating system. Recognizing this dynamic, premier institutions like Menninger and Hazelden mandate family engagement, often structuring it around virtual sessions or intensive on-site “Family Weeks.”Addiction thrives in isolation and secrecy; recovery requires a restructuring of the family dynamic.
Clinical Outlook
The era of the “28-day spin dry” is ending. The data is irrefutable: addiction is a chronic, relapsing condition, much like Type 2 Diabetes or Hypertension. It requires long-term management, not a one-time fix.
In 2026, the best centers are those that plan the discharge on the day of admission. They are building a scaffold that extends months into the future—connecting the patient to outpatient psychiatrists, sober living environments, and recovery coaching.
For the family searching today: ignore the sponsored ads promising a cure in paradise. Start with the boring, clinical indicators of quality. The Joint Commission seal is your first green light. From there, dig into the outcomes data and scrutinize the doctors’ credentials. Recovery is not a luxury product; it is a medical discipline. Choose the hospital, not the hotel.
References:
1. American Society of Addiction Medicine. ASAM Criteria, Fourth Edition. ASAM. Accessed February 13, 2026. https://www.asam.org/asam-criteria/asam-criteria-4th-edition
2. The Menninger Clinic. Treatment Outcomes. The Menninger Clinic. Accessed February 13, 2026. https://www.menningerclinic.org/why-menninger/treatment-outcomes
3. Hazelden Betty Ford. Addiction Treatment Patient Outcomes: Tracking Results. Hazelden Betty Ford. Published July 22, 2024. Accessed February 13, 2026. https://www.hazeldenbettyford.org/press-release/patient-outcomes
4. Addiction Help. Avoiding Patient Brokering: AKS & Stark Law Guide. Addiction Help. Published December 31, 2025. Accessed February 13, 2026. https://www.addictionhelp.com/for-providers/avoiding-patient-brokering
5. The Joint Commission. Behavioral Health Care & Human Services Accreditation Program. The Joint Commission. Accessed February 13, 2026. https://www.jointcommission.org/en-us/accreditation/behavioral-health-care-and-human-services
Disclaimer: This article is intended for informational purposes only and does not constitute medical advice. Ultimately, always consult with a qualified healthcare professional for any health concerns. Consequently, please prioritize this step before making any decisions related to your health or treatment.
