The Metabolic Shield
Michelle Robinson, a 45-year-old woman, did not fit the stereotype of a cardiac patient. She wasn’t old, and she didn’t spend her days in a recliner. Yet, when the dull pain in her chest escalated, she found herself in an emergency room facing a diagnosis that seemed impossible: a heart attack caused by an artery that was 90% blocked.
Her survival was just the first hurdle. The second was the psychological abyss that opened up after discharge. “The hospital literally said, ‘You’re free to go home. Follow up with the cardiologist.’ It’s kind of wild,” Robinson told the American Heart Association (AHA). She felt abandoned, terrified that any movement might trigger another event. She represents a critical demographic in the United States: adults navigating the terrifying gap between a chronic diagnosis and the lifestyle changes required to survive it.
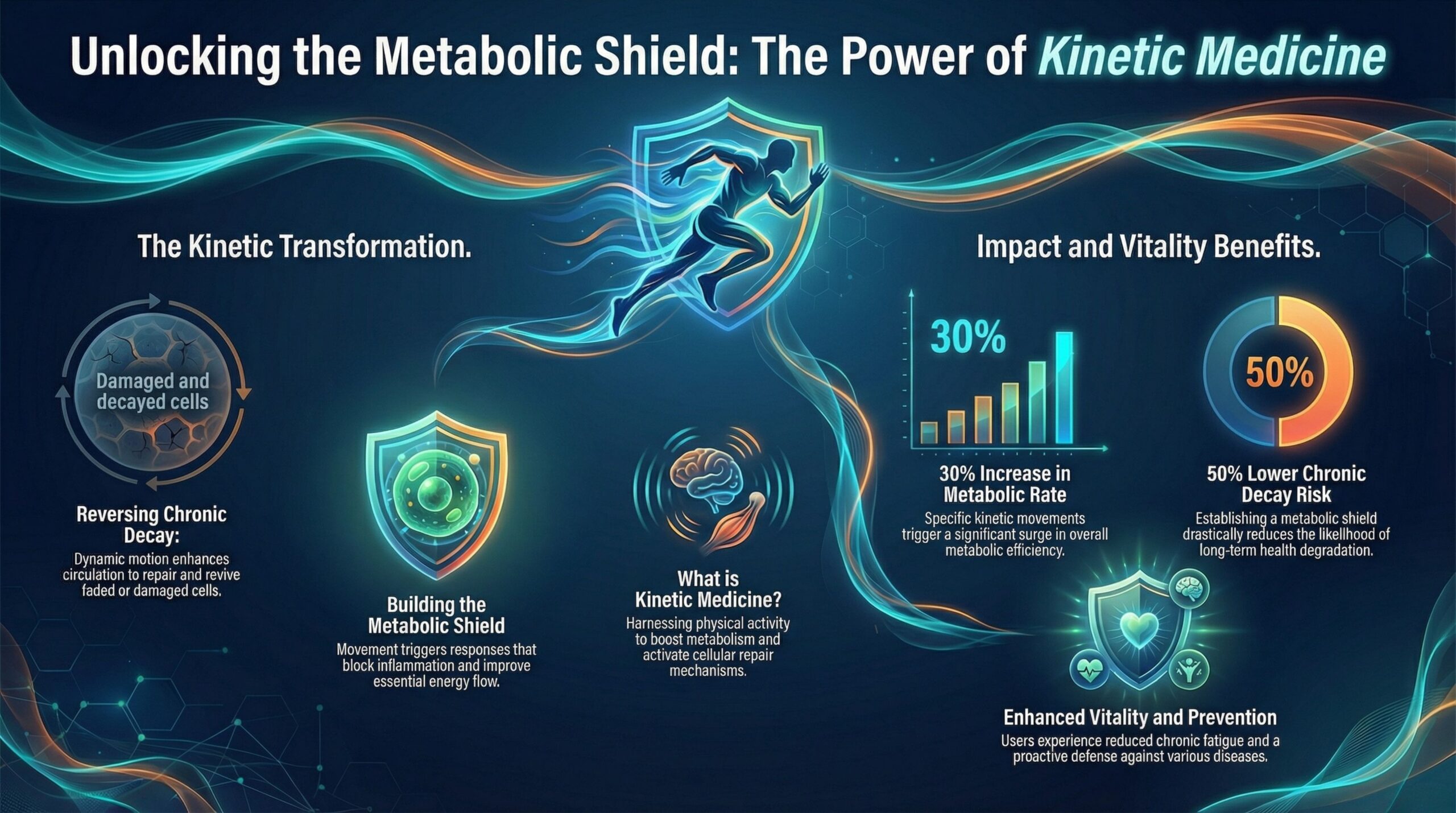
Robinson’s turning point came not from a pill bottle, but from a referral to cardiac rehabilitation—a medically supervised program that treats exercise not as a hobby, but as a prescription drug. This distinction is vital. In the clinical landscape of 2026, physical activity is no longer viewed merely as a tool for weight loss; it is recognized as “kinetic medicine,” a physiological intervention capable of remodeling arterial walls and reprogramming cellular metabolism.
The Physiology of Kinetic Medicine
To understand why exercise saves lives like Robinson’s, we must strip away the gym marketing and look at the molecular machinery. The human body is not designed for the sedentary environments we have constructed. When muscles contract, they do far more than move bone; they act as a massive endocrine organ.
Skeletal muscle, the largest organ in the body by weight, releases signaling molecules called myokines during contraction. These myokines travel through the bloodstream, communicating with the liver, adipose tissue (fat), and the brain. They reduce systemic inflammation—the root cause of both atherosclerosis (plaque buildup) and insulin resistance.
When a patient remains sedentary, this signaling network goes silent. The “metabolic shield” drops. Glucose lingers in the bloodstream, caramelizing proteins (glycation), while endothelial cells in the arteries stop producing nitric oxide, causing vessels to stiffen. The result is a slow, silent progression toward catastrophe.
Case Study: The Diabetes Prevention Paradigm
The most compelling evidence for exercise as a frontline treatment comes from the landmark Diabetes Prevention Program (DPP), a clinical trial that fundamentally changed how physicians view Type 2 diabetes.
Consider the case of Jan Booker, a 60-year-old medical librarian profiled by the CDC. Like millions of Americans, Booker faced a “pre-diabetes” diagnosis—her blood glucose levels were elevated (likely between 100 and 125 mg/dL), signaling that her pancreas was struggling to keep up with demand.
The standard medical response might have been to wait until she developed full-blown diabetes and then prescribe Metformin. However, the DPP outcomes showed that a structured lifestyle intervention was significantly more effective than Metformin. Participants who lost just 7% of their body weight and engaged in 150 minutes of moderate activity weekly reduced their risk of developing Type 2 diabetes by 58%. For those over age 60, like Booker, the risk reduction was an astounding 71%.
The Mechanism: The GLUT4 “Back Door”
Why is exercise so potent for patients like Booker? The answer lies in a protein called GLUT4 (Glucose Transporter Type 4).
In a healthy body, insulin acts like a key, unlocking cells to let glucose in. In Type 2 diabetes, the lock is jammed (insulin resistance). Exercise, however, bypasses this lock entirely. Muscle contraction activates an enzyme called AMP-activated protein kinase (AMPK). This enzyme triggers GLUT4 transporters to move to the cell surface *without* the need for insulin.
Effectively, exercise opens a “back door” for glucose to enter muscle cells. This effect persists for up to 48 hours after a workout, which is why consistency is clinically more important than intensity for diabetic management. By riding her bike and altering her diet, Booker didn’t just “burn calories”; she mechanically forced her muscles to clear glucose from her blood, eventually reversing her pre-diabetic state.
The Heart: Remodeling the Engine
For cardiac patients like Michelle Robinson, the stakes are immediate. The fear of exercise after a heart attack is rational—patients worry that elevating their heart rate will cause another blockage. However, physiology dictates the opposite.
Shear Stress and the Endothelium
The inner lining of blood vessels, the endothelium, is highly sensitive to the flow of blood. When a person exercises, blood flow increases, creating “shear stress” against the vessel walls. This physical force stimulates endothelial cells to produce nitric oxide, a gas that relaxes the vessels (vasodilation) and prevents platelets from sticking to the walls.
Furthermore, chronic exercise promotes “collateralization.” If a main coronary artery is slowly narrowing, regular aerobic stress signals the heart to grow new, smaller blood vessels to bypass the blockage—a natural double bypass.
In Robinson’s case, cardiac rehab provided a controlled environment where she could safely elevate her heart rate. The program didn’t just rebuild her cardiovascular capacity; it rebuilt her psychological resilience. “It’s not just physical recovery, it’s really mental recovery,” she noted. She lost 20 pounds, but more importantly, she regained the confidence that her heart was an engine capable of repair, not a ticking time bomb.
The Reality Check: When Lifestyle Fails
While the benefits are clear, the clinical reality is often messier. It is crucial to address the limitations of lifestyle interventions to maintain an honest dialogue.
The “Look AHEAD” (Action for Health in Diabetes) trial serves as a sobering counter-narrative. This massive study followed over 5,000 adults with Type 2 diabetes to see if intensive lifestyle intervention could reduce heart attacks and strokes. The trial was stopped early for “futility”—meaning the lifestyle group did not have fewer cardiovascular events than the control group.
Does this mean exercise doesn’t work? No. It highlights that once metabolic damage is advanced, reversing cardiovascular risk is incredibly difficult. However, a secondary analysis of the Look AHEAD data revealed a crucial nuance: participants who managed to lose at least 10% of their body weight *did* see a 21% reduction in mortality.
This data suggests a “dose-response” relationship. Dabbling in exercise is insufficient for patients with established disease. To reverse the trajectory of chronic illness, the intervention must be significant, sustained, and often aggressive.
Clinical Protocol: The Professional Standard (US Context)
So, what is the correct “dose”? In the United States, the American College of Sports Medicine (ACSM) sets the gold standard for clinical exercise prescription.
We spoke with clinical exercise physiologists who adhere to the 2025 ACSM guidelines. For an adult seeking to prevent or manage chronic disease, the “walk around the block” advice is often inadequate. The prescription must follow the F.I.T.T. principle (Frequency, Intensity, Time, Type).
1. The Glucose Control Protocol (Diabetes/Pre-diabetes)
- Frequency: Daily is optimal. Never skip more than two consecutive days, as the insulin-sensitizing effect of exercise wears off after 48 hours.
- Intensity: Moderate-to-Vigorous. You should be able to talk, but not sing. (RPE 12-13 on a scale of 6-20).
- Time: 150 minutes per week minimum.
- Type: A combination of aerobic activity and resistance training.
- Crucial Update: The 2024 ACSM consensus emphasizes “breaking sedentary time.” Sitting for 4 hours negates many benefits of a 30-minute workout. Patients are advised to perform “movement snacks”—2 minutes of walking or squatting every 30 minutes.
2. The Cardiac Protection Protocol (Hypertension/Post-Event)
- Frequency: 3-5 days per week.
- Intensity: Zone 2 training (60-70% of max heart rate). This keeps the heart below the threshold where stress hormones (catecholamines) spike excessively.
- Resistance: Light-to-moderate weights. Warning: Patients with uncontrolled hypertension (BP > 160/100 mmHg) must avoid heavy lifting and the “Valsalva maneuver” (holding breath), which can cause dangerous spikes in blood pressure.
The Trainer’s Perspective: Bridging the Gap
“The biggest mistake I see is the ‘Weekend Warrior’ mentality,” says a certified Clinical Exercise Physiologist (CEP) based in Chicago (name withheld for privacy). “Patients do nothing Monday through Friday, then try to run a 10K on Saturday. For a diabetic or cardiac patient, this is dangerous. We need ‘chronic’ exercise to fight chronic disease.”
Professional trainers in the US are increasingly moving toward “hybrid training”—mixing steady-state cardio with resistance training.
- Resistance Training is Non-Negotiable: Muscle mass is the primary disposal site for blood glucose. Sarcopenia (muscle loss) is a direct risk factor for diabetes mortality. Even two sessions of resistance training a week can improve insulin sensitivity by 46%.
- Safety First: For diabetic patients, trainers must check for foot ulcers (neuropathy) and ensure footwear is specialized. For cardiac patients, heart rate monitors are mandatory during the initial phases of training.
Clinical Prognosis
The narrative of chronic disease in America is often written as a tragedy of inevitability: diagnosis, medication, decline. But cases like Jan Booker and Michelle Robinson rewrite that script. They demonstrate that the human body retains a remarkable capacity for plasticity well into adulthood.
However, the “pill” of exercise is difficult to swallow. It requires time, effort, and often a complete restructuring of one’s life. The barriers—lack of walkable cities, time poverty, and the intimidation factor of gyms—are real and potent.
The medical community is shifting. We are moving away from vague advice (“eat less, move more”) toward precise, monitored prescriptions (“walk 30 minutes at 3 mph, 5 times a week, after meals”). This precision medicine approach turns the patient from a passive recipient of healthcare into an active participant in their own rescue.
For the 45-year-old staring at a ceiling, wondering if their life is over, the science ultimately offers a definitive answer. In fact, the biology of repair is waiting. It just needs the signal to start.
References & Further Reading:
1. Diabetes Prevention Program Research Group. (2002). “Reduction in the Incidence of Type 2 Diabetes with Lifestyle Intervention or Metformin.” New England Journal of Medicine.
2. Look AHEAD Research Group. (2013). “Cardiovascular Effects of Intensive Lifestyle Intervention in Type 2 Diabetes.” New England Journal of Medicine.
3. Kanaley, J. A., et al. (2022). “Exercise/Physical Activity in Individuals with Type 2 Diabetes: A Consensus Statement from the American College of Sports Medicine.” Medicine & Science in Sports & Exercise.
4. Centers for Disease Control and Prevention (CDC). (2024). “National Diabetes Prevention Program: Real People, Real Stories.”
5. American Heart Association (AHA). (2023). “Cardiac Rehab Patient Stories: Michelle Robinson.” Next Avenue / AHA.
6. Sylow, L., et al. (2017). “Exercise-stimulated glucose uptake — regulation and implications for glycaemic control.” Nature Reviews Endocrinology.
Disclaimer: This article is intended for informational purposes only and does not constitute medical advice. Ultimately, always consult with a qualified healthcare professional for any health concerns. Consequently, please prioritize this step before making any decisions related to your health or treatment.
