Joint Pain Relief for Seniors: A Guide to Natural and Medical Options
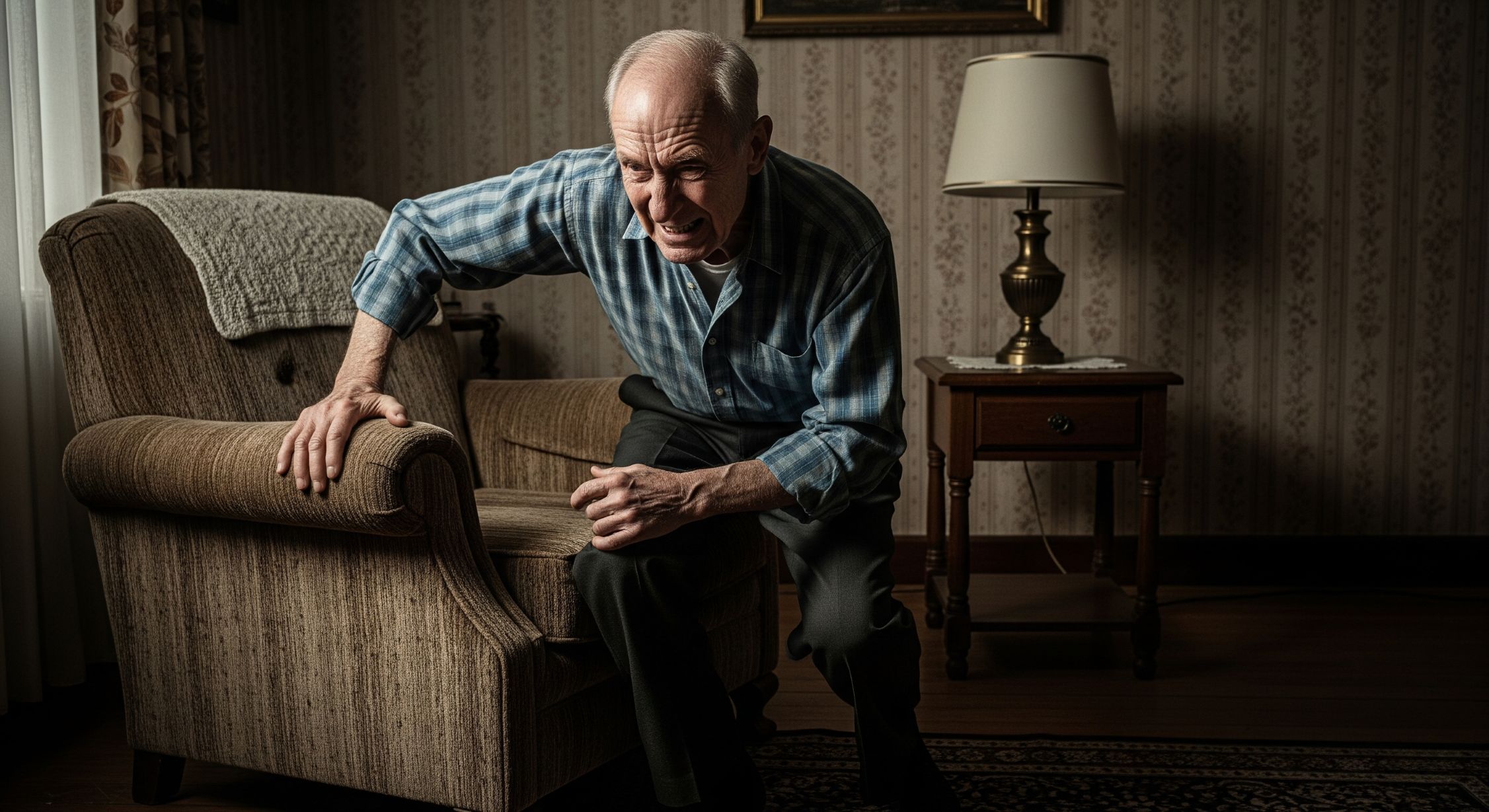
Joint pain is a common companion for many people as they age. It can range from a mild ache to a debilitating throb that makes everyday activities a challenge. While it is a widespread issue, you should know that it is not something you have to simply endure. A wide array of effective strategies exist to manage and alleviate joint pain, ranging from natural, lifestyle-based changes to advanced medical treatments. This comprehensive guide, therefore, explores these options in detail, providing a roadmap for seniors seeking to reclaim their mobility and improve their quality of life.
Understanding the Causes of Joint Pain in Seniors
Before you can effectively manage joint pain, it is crucial to understand its origins. The most common cause is osteoarthritis (OA), often referred to as “wear-and-tear arthritis.” Over time, the cartilage that cushions the ends of your bones deteriorates. As a result, bones begin to rub directly against one another, causing pain, stiffness, and swelling. This is particularly prevalent in weight-bearing joints like the knees, hips, and spine. Furthermore, a more serious, but less common, cause is rheumatoid arthritis (RA). In this condition, your body’s immune system mistakenly attacks the lining of your joints. Ultimately, this causes chronic inflammation and can lead to joint deformity and bone erosion. Other causes include gout, bursitis, and old injuries. The key takeaway, then, is that different types of pain require different treatment approaches. Therefore, a proper diagnosis from a healthcare professional is your first and most important step.
“More than 32.5 million adults in the United States have osteoarthritis. This is the most common form of arthritis.” – Centers for Disease Control and Prevention (CDC)
The Power of Natural and Lifestyle-Based Approaches
Many seniors prefer to start their journey toward pain relief with natural methods. These options often carry fewer side effects and can be incredibly effective when used consistently. Moreover, they empower you to take an active role in your own health.
1. The Anti-Inflammatory Diet
What you eat directly impacts your body’s inflammatory response. Consequently, choosing the right foods can significantly reduce joint pain. A diet rich in anti-inflammatory foods and low in pro-inflammatory items can make a huge difference. You should focus on foods rich in omega-3 fatty acids, such as fatty fish like salmon, mackerel, and sardines. You can also find them in flaxseeds, walnuts, and chia seeds. In addition, consume plenty of leafy green vegetables, like spinach and kale, which are loaded with antioxidants. For cooking, use extra-virgin olive oil and coconut oil, which possess natural anti-inflammatory properties. To season your meals, use spices like turmeric and ginger. Turmeric, for instance, contains a powerful compound called curcumin, which many studies show can reduce joint pain and inflammation. Ginger also offers similar benefits.
“Anti-inflammatory diets emphasize fruits, vegetables, lean protein, nuts, seeds, and healthy fats while limiting foods that promote inflammation.” – Johns Hopkins Medicine
On the other hand, it is equally important to limit foods that promote inflammation. These include processed foods, sugary snacks and beverages, and refined carbohydrates like white bread and pastries. Trans fats and saturated fats, found in fried foods and red meat, can also worsen inflammation. By prioritizing a clean, whole-food diet, you give your body the tools it needs to fight inflammation from within. This foundation is, therefore, essential for long-term joint health.
2. The Role of Exercise and Physical Activity
It may seem counterintuitive, but movement is one of the best things for painful joints. Exercise strengthens the muscles around your joints, providing crucial support and reducing stress on the cartilage. It also helps lubricate your joints, improves flexibility, and reduces stiffness. The key is to choose low-impact activities that don’t put excessive stress on your joints. Activities like walking, swimming, and cycling are excellent choices. Walking, for example, improves circulation and joint flexibility without harsh impact. Swimming and water aerobics are particularly beneficial because the water’s buoyancy supports your body weight, drastically reducing pressure on your joints. Another great option is strength training. Strengthening your muscles can offload stress from your joints. You don’t need heavy weights; use resistance bands or light dumbbells to target key muscle groups around your knees, hips, and shoulders. In addition, gentle stretching from activities like yoga or tai chi can improve your range of motion and flexibility. These exercises also help with balance, which is crucial for preventing falls and subsequent injuries.
“Exercise helps you lose weight, strengthens the muscles around your joints, and keeps joints lubricated. This can lead to less pain and better joint function.” – Arthritis Foundation
A physical therapist can also create a personalized exercise plan tailored to your specific condition and pain level. This will ensure you are performing exercises safely and effectively.
3. Natural Supplements
Many people turn to dietary supplements to complement their diet and exercise routines. While results can vary, some supplements show promise for joint health. For example, Glucosamine and Chondroitin are natural components of healthy cartilage. Supplementing with them can, in some cases, help reduce pain and slow the progression of cartilage degeneration. For some individuals, they may provide significant relief. If you don’t consume enough fish, you can take fish oil supplements. They offer the same powerful anti-inflammatory benefits as the fatty fish they come from. Another promising supplement is MSM (Methylsulfonylmethane), a compound that can reduce pain and swelling, as well as improve physical function. Many joint health supplements contain it as a key ingredient. Finally, you can take turmeric and ginger in supplement form, which gives you a more concentrated dose of their active compounds, curcumin and gingerols.
“Glucosamine and chondroitin are natural compounds found in healthy cartilage. Some studies suggest that supplements may help with osteoarthritis pain and function.” – Mayo Clinic
Before starting any supplement, you should always consult your doctor. They can advise you on the correct dosage and ensure the supplement won’t interact negatively with any medications you are taking.
Medical and Pharmacological Options
For more severe or persistent joint pain, medical intervention often becomes necessary. A healthcare provider can recommend a range of effective treatments, from over-the-counter medications to surgical procedures.
1. Over-the-Counter (OTC) Pain Relievers
These are often the first line of defense against mild to moderate joint pain. For instance, Acetaminophen (Tylenol) works by changing how your body perceives pain. It is generally safe for most people when taken at the recommended dose. However, you must avoid taking more than the daily limit, as it can cause liver damage. Likewise, Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) like ibuprofen (Advil, Motrin) and naproxen (Aleve) reduce both pain and inflammation. While highly effective, long-term use can cause stomach irritation, kidney problems, or an increased risk of heart issues. Your doctor will advise you on the best and safest way to use them.
“NSAIDs block the production of certain chemicals that cause inflammation and pain. They can be very effective for joint pain and swelling.” – Cleveland Clinic
2. Prescription Medications
When OTC options are not enough, a doctor may prescribe stronger medications. One option is Topical NSAIDs. Gels and creams containing NSAIDs can provide targeted pain relief without the systemic side effects of oral medications. These are a great option for people with pain in a specific joint. Another medication, Duloxetine (Cymbalta), was originally an antidepressant. However, doctors also use it to treat chronic pain, including pain from osteoarthritis. Finally, your doctor can inject Corticosteroids, which are powerful anti-inflammatory drugs, directly into the affected joint. This can provide rapid and significant pain relief for weeks or even months. Note, however, that the effects are temporary, and repeated injections are not recommended.
3. Physical Therapy and Rehabilitative Care
A physical therapist is a key partner in managing chronic joint pain. They work with you to create a personalized plan, which includes exercises to improve strength, flexibility, and range of motion. A physical therapist will also use hands-on techniques to reduce pain and swelling. Moreover, they will teach you proper body mechanics to protect your joints from future injury.
“Physical therapy is often a core component of a treatment plan for chronic joint pain. A therapist helps you learn exercises to reduce pain and improve flexibility and function.” – WebMD
4. Injections for Joint Pain
Beyond corticosteroids, other types of injections can provide relief. First, Hyaluronic Acid Injections involve a component of the fluid that lubricates your joints. Injecting it can help improve lubrication and reduce pain, particularly in the knee. The effects can last for several months. Second, Platelet-Rich Plasma (PRP) Therapy is an experimental treatment that involves taking a sample of your blood, concentrating the healing platelets, and injecting them into the joint. Doctors believe the growth factors in the platelets can help repair damaged tissue.
“PRP therapy has gained popularity for treating orthopedic conditions and joint pain, as it utilizes the body’s own healing properties to promote tissue repair.” – Duke Health Orthopedics
5. Surgical Options: The Last Resort
When all other treatments have failed and a patient’s quality of life is severely impacted, a doctor may recommend surgery. For example, for severe arthritis in the knee or hip, a surgeon can perform Joint Replacement Surgery (Arthroplasty). During this procedure, the damaged joint is removed and replaced with a prosthetic one made of metal or plastic. This is a major surgery; however, it can provide permanent relief from pain and restore function for many years. Recovery, as you might expect, involves intensive physical therapy.
“A total knee replacement can provide dramatic pain relief and restore function in people with severe arthritis.” – Cedars-Sinai
A Holistic Approach: Combining Strategies for Optimal Relief
The most effective plan for managing joint pain often involves a combination of both natural and medical strategies. A holistic approach recognizes that your body and mind are interconnected. This can include a focus on things like stress management and improving sleep quality. For example, a person with osteoarthritis might start their day with a brisk walk. Following their workout, they might take an NSAID to manage any discomfort. Throughout the day, they focus on eating a diet rich in anti-inflammatory foods. In the evening, they may apply a topical cream and use a heating pad to soothe stiff joints.
For long-term management, they regularly meet with a physical therapist and take a daily supplement. If, despite these efforts, they experience a severe flare-up, a doctor might recommend a corticosteroid injection to provide temporary relief.
“A multi-disciplinary approach to pain management, which includes both medical treatments and lifestyle modifications, often yields the best results for chronic conditions like arthritis.” – Hospital for Special Surgery (HSS)
Ultimately, your journey to joint pain relief is unique. For this reason, you should always work closely with your healthcare team—your doctor, physical therapist, and possibly a registered dietitian. Together, you can create a personalized and comprehensive plan that targets the root causes of your pain and gives you the tools to live a more active and comfortable life.
Conclusion: Taking Control of Your Health
Joint pain in seniors is a complex issue, but it is certainly manageable. By understanding its causes and exploring the vast range of available options, you can take control of your health. Start with lifestyle changes, focusing on a healthy diet and regular, low-impact exercise. Supplement these efforts with over-the-counter pain relievers or natural supplements as needed. If pain persists, do not hesitate to seek medical advice for more targeted treatments. By combining these strategies, you can reduce discomfort, improve your mobility, and significantly enhance your overall quality of life. The path to relief is a journey, but it is one you can successfully navigate with the right knowledge and a proactive mindset.
Sources
- Centers for Disease Control and Prevention (CDC)
- Johns Hopkins Medicine
- Arthritis Foundation
- Mayo Clinic
- Cleveland Clinic
- WebMD
- Duke Health Orthopedics
- Cedars-Sinai
- Hospital for Special Surgery (HSS)